Retirement Life
28 April 2025
A lifelong commitment to aged care
Aged Care Commissioner Carolyn Cooper grew up in a three-generational household, and her children have enjoyed the same. It’s fostered a deep interest in fighting to improve life and health outcomes for older people. She chats to us about her life and her current role.
Can you share some background on yourself and how you came to this role?
I'm a farm girl from the Wairarapa and did my nursing training many, many years ago, working through lots of different clinical fields. But I always had a desire to improve patient outcomes in a broader sense, rather than just the patient in front of me.
I also grew up in a really cool environment with lots of older people around me. So I've always had an interest in older people.
I worked in senior executive roles across New Zealand and Australia and when I came back to New Zealand from Australia, I spent five years with Bupa Villages in aged care - and ended up as managing director. I became the Aged Care Commissioner three years ago.
Tell us a bit about your role as Aged Care Commissioner
It's an inaugural role and it's independent, sitting in the Office of the Health and Disability Commissioner. However, I'm also a deputy commissioner under the Health and Disability Commissioner legislation. So, from a health and disability perspective, I'm a decision maker on complaints and on ensuring that the Code of Consumer Rights is upheld for all consumers across Aotearoa.
As Aged Care Commissioner, I have a particular focus on improving the quality of care for older people, the quality of health and disability services for older people and also providing strategic leadership to the health and disability sector.
The complaints that come into the Office of the Health and Disability Commissioner help to inform my focus on making recommendations for improvement.
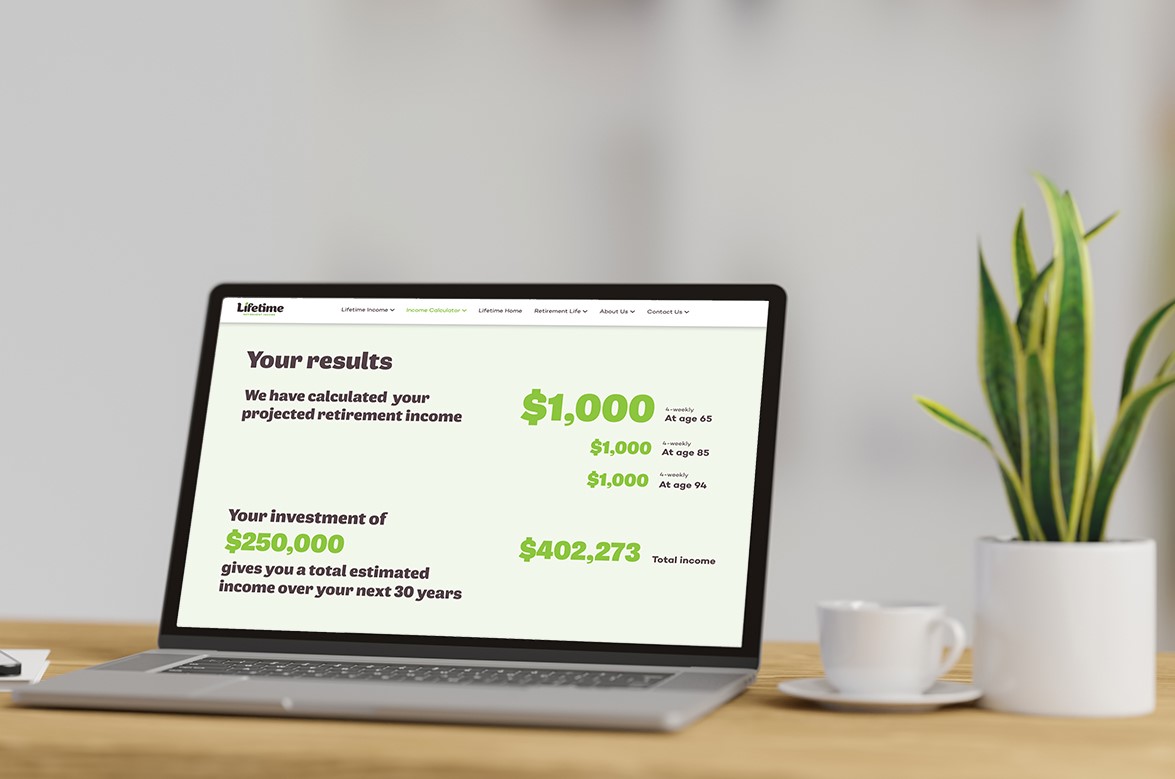
Calculate what you could draw in retirement.
What are the most significant issues you’re dealing with currently, and how is the Commission working to make a difference?
The intent in the health system is still incredible around caring and compassion. From an individual perspective, there are incredible things happening all the time - but the broader system is under pressure and older people are feeling that.
The issues for older people are largely the same as they have been for a long time - which is a challenge and a disappointment really. There's a need for the health system to look at older people across the entire healthcare continuum. So ensuring that primary and community care services are really focused on older people, on keeping them well and out of hospital. Then if people do go into hospital, that they get access when they need it and then have as short a stay as possible.
If they need home and community support and/or aged residential care, they need to have access to that as quickly as possible as well. That’s the challenge, there isn't really a coordinated approach to strategic health services for older people across the entire system.
There are also still concerns about the themes that we see in the care of older people. Such as challenges around escalating the care needs of deteriorating older people appropriately and in a timely way. But the good thing is some amazing work has been done on a deteriorating early warning system (DEWS) for Aged Residential Care. It’s a tool that will assist staff with their assessment of unwell residents.
I work with the key people who do have influence over the system such as Ministers, the Ministry of Health, Te Whatu Ora, Health New Zealand, and other agencies like the Aged Care Association and the Home and Community Health Association, to try and influence change that way.
Also, when a complaint comes in that requires a recommendation to improve care, we make those recommendations, and they’re monitored. If people don't comply, we continue to work with them until they do. We shine a spotlight on different aspects of the health system to try and ensure there is improvement.
What one issue keeps you up at night?
If we could ensure we were supporting older people in different ways to keep them out of public hospitals, for instance, or get them home much quicker, that would make a real difference. That’s what keeps me awake at night.
The highest and fastest growing proportion of the population is those in the over-75 and over-85 age brackets. Older people are the highest users of the health system, and therefore the highest cost.
It's about investing in the system outside of the acute areas to prevent people needing acute care, and when they do, for them to have more streamlined opportunities to get home. I know that many older people stay in hospital for longer than they either need to or want to because they can't access home and community support services. So they stay in the wrong part of the health system. Patient flow is one of the key things that needs to be looked at.
There also needs to be longer-term contracts for health services. I think it needs to be one of the things that whichever government is leading this country ensures we actually have some continuity around the approach and the strategy - that it's not impacted by government changes all the time. And that the health system is seen as a really important area and investment considered around the continuum of healthcare, the value for money, for older people particularly, but for all of us. Because every time we have someone stuck in the wrong part of the health system, it impacts us all.

Aged Care Commissioner Carolyn Cooper
Does this lack of continuity of care include access to aged residential care?
There are plenty of aged residential care beds across New Zealand, but regionally and rurally, sometimes there's not the right type of bed in the right place. So it's a distribution issue rather than a volume issue for the current population numbers.
What is one piece of advice would you give those nearing/in retirement?
Look after the things you can influence with your own health. Focus on prevention. There are three areas that we're encouraging older people to focus on this year. Hearing health, because of the risks associated with poor hearing and dementia. Oral health, again because of the impact on your health if your teeth are not healthy. And then bone health, so that you're less likely to end up with a fracture.
The last thing would be to absolutely and utterly stay connected to your networks, because loneliness is very negative to your health.
Who inspires you most in the retirement/ageing arena?
Well, the inspiration to me was my Mum. I went into the Bupa aged care role because my mum had gone into aged residential care, and I thought I could add some value to that system. So older people are my inspiration, particularly my mum, but also other members of my broader whānau as well.
What’s the number one thing you would like to spend more time doing in retirement yourself one day?
Time with my family and friends, because that's the challenge when you've been doing big jobs - you don't have as much family and friend time.
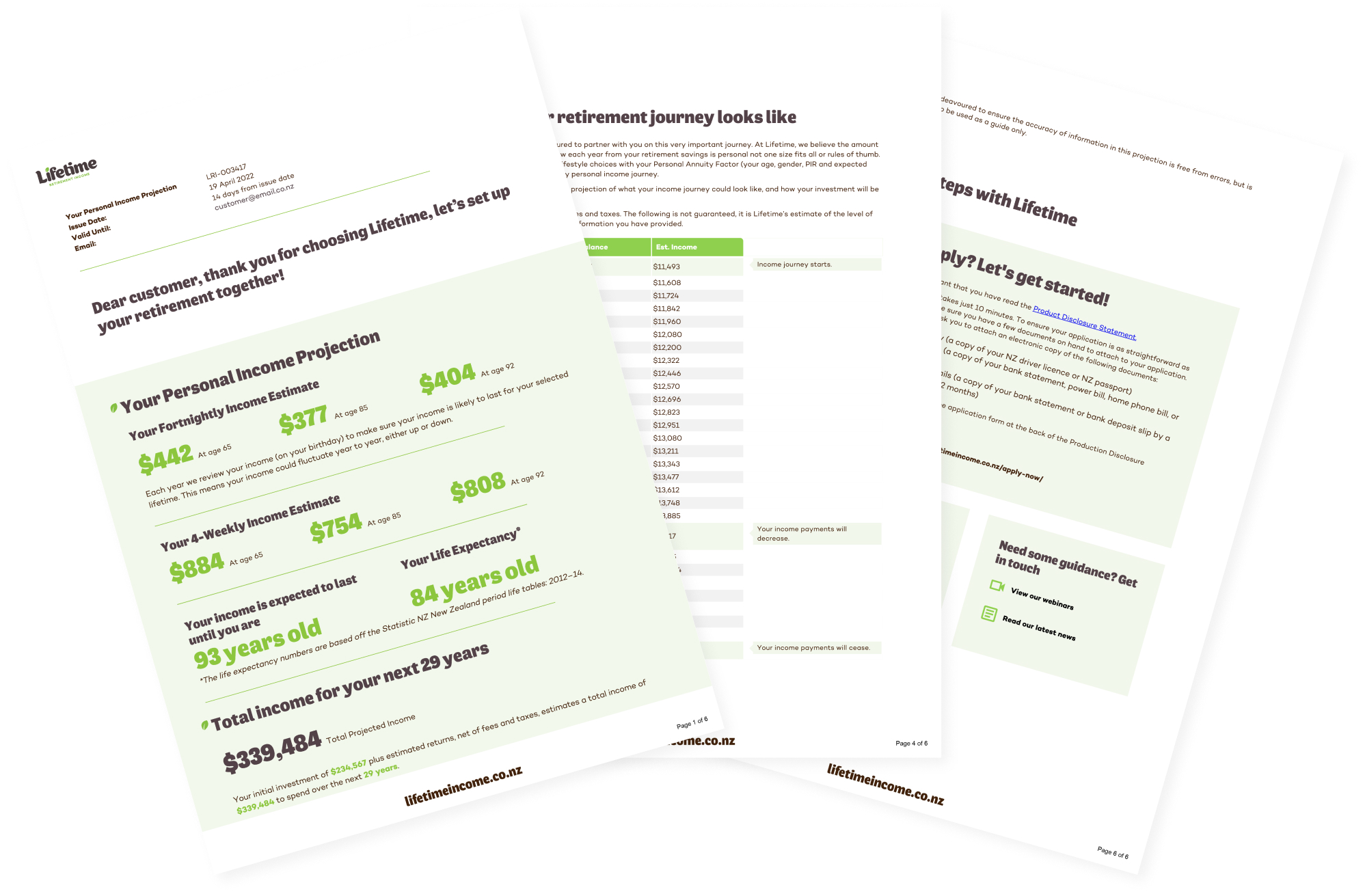
Project your retirement income.
Invest with Lifetime for a retirement income managed for living.
