Retirement Life
3 September 2025
Profile: Gretchen Leuthart, Hospice New Zealand
Dying is a life stage that we often fail to recognise or honour, leaving us unprepared for it, says Hospice New Zealand communications manager Gretchen Leuthart. She shares her insights on how we can die better.
Please share some background on yourself and how you came to work for Hospice NZ?
My Mum died at home 14 years ago, in the care of Hospice Taranaki. I was so struck by the holistic, whole-of-person care hospice provided. Not only were Mum’s physical symptoms managed but her fears and hopes were addressed and her concerns for the people she loved. She died peacefully as a result, and I knew I wanted to contribute to this amazing movement.
I was lucky that the perfect job came up. I’ve spent my career in communications and marketing but lately I’ve been drawn to the community sector where I can use my skills to advocate for social good – equitable palliative care for all New Zealanders is definitely in that camp!
What changes have you noticed regarding the issues and challenges faced by Hospice NZ over your time with them?
I’ve been with Hospice NZ for nearly four years. Sadly, in my time not much has changed in that the major issue facing the sector is still underfunding from the government. This has placed an unsustainable burden on community fundraising to fill the gap in order to keep hospice services for dying people free.
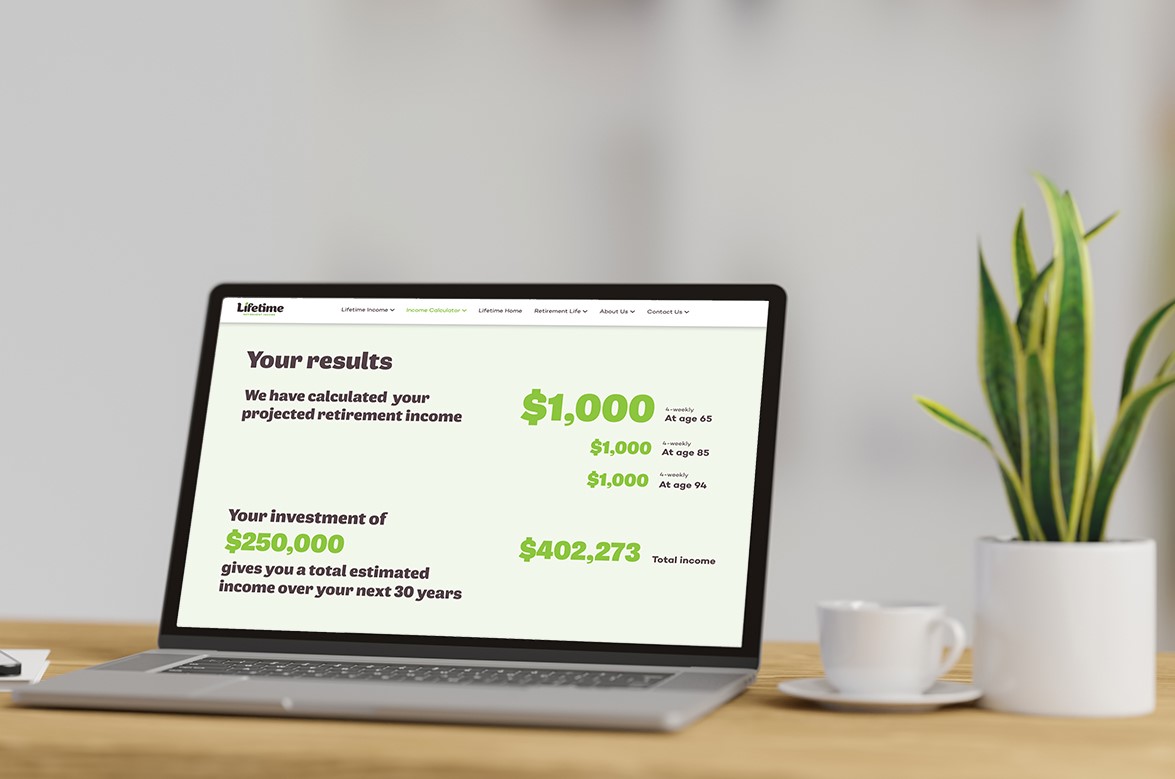
Calculate what you could draw in retirement.
Hospice is an essential service that we all hope will be there when we need it. Last year, it cost $226 million to run the country’s hospice services, but the government only provided $114 million. Hospices raised $112 million from community donations, fundraising, and other sources just to keep going.
The demand for hospice care continues to rise. Last year, hospice cared for over 19,000 people and their families, and as our population grows older and lives longer, it’s predicted that the number of people needing palliative care will increase by 50 per cent by 2040.
The challenge is that without fairer, sustainable funding from government, we just won’t meet the current, let alone future, need for quality end-of-life care.
What do you wish people better understood about dying and how they can prepare for it?
In New Zealand, close to 40,000 people die each year, and most of these are not sudden. People can be living while dying, or in other words, with a terminal illness for weeks, months and years. But as a stage of life, dying is not often recognised or honoured, and as a result, we don’t prepare for it.
We can prepare by talking about it more, having open and honest conversations about what we hope, what we fear, what we don’t understand, and what we’d like to know more about. We can fill out an Advanced Care Plan (this is a great tool where you write down what you value, your concerns and what your care preferences are when you are dying). We can build up our death literacy by finding out about palliative care options in our region. Hospice is not just for the final few days; in fact, people who receive hospice care earlier in their dying journey feel more prepared and accepting and experience a sense of well-being.
I think in undervaluing this life stage, we often forget to support the carers looking after the dying too. Caregivers, most often family members, need space to grieve, rest, and be supported as well. To better support dying as a life stage, our society needs to see dying as a normal process.

Gretchen Leuthart: Hospice New Zealand Communications Manager
What does ‘dying well’ look like and how can people work it for themselves and those they love?
I love how palliative care physician and author, Dr Ira Byock, pictures this: “When a person is well within themselves, with the world, with the people they love, with their God, or the Universe or nature, as they are leaving this life.”
Dying is part of living. Of course, it’s hard and not wanted, but there is still human potential and value in this stage, and with palliative care and a compassionate community around you, I believe it can be a rich time of life that includes a sense of well-being.
Please tell us a little about the TV show Hospice Heroes that’s currently available
This show takes an intimate look inside Tōtara Hospice in South Auckland. You see the joy, laughter and life that goes on daily even in the face of death. It is helping demystify hospice and end-of-life care. You see that it isn’t about the building, but about the doctors, nurses, allied staff and volunteers at the heart who uplift the patients and families every day. It reminds us that we can live every moment until the end. It's streaming on TV3Now.
If you could give your younger self one piece of retirement/aging advice, what would it be?
Cherish and hold on to your friends. Having social connections and friendships is so important for us in order to age well and to die well.
What’s the number one thing you would like to spend more time doing in retirement yourself one day?
I hope I’ll be volunteering for a hospice. I’d especially love to help with the Biography service that many hospices offer. Helping to record someone’s life as they reflect and review their life experience would be such a privilege.
Project your retirement income.
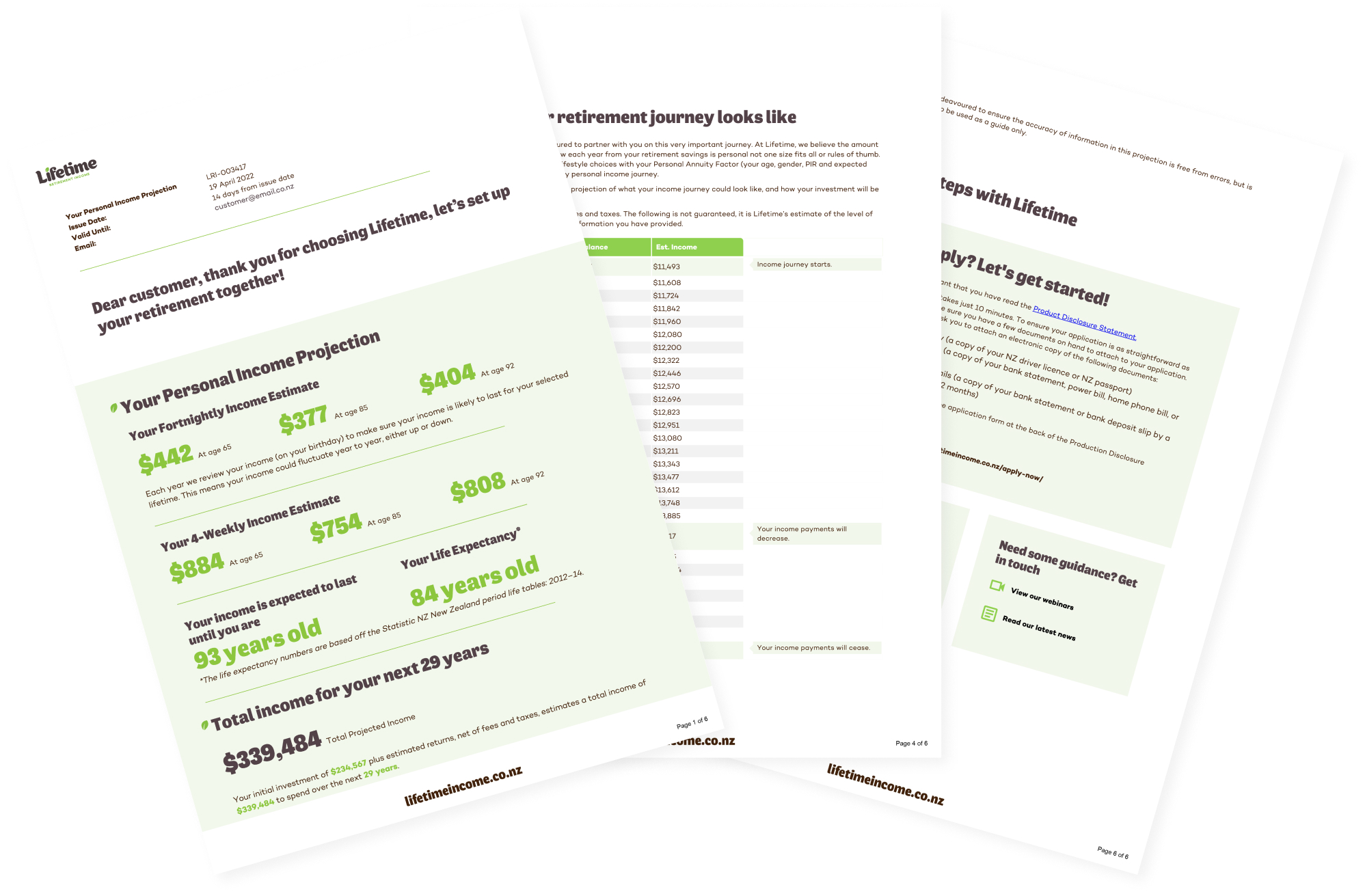
Invest with Lifetime for a retirement income managed for living.
